Understand SMA
What is SMA
SMA is characterised by a loss of important cells in the spinal
cord called motor neurons. Over time, the breakdown of these
neurons leads to a gradual decline in muscle size and strength.
While primarily a childhood condition, SMA can be diagnosed
in adolescents, and sometimes beyond 18 years of age.
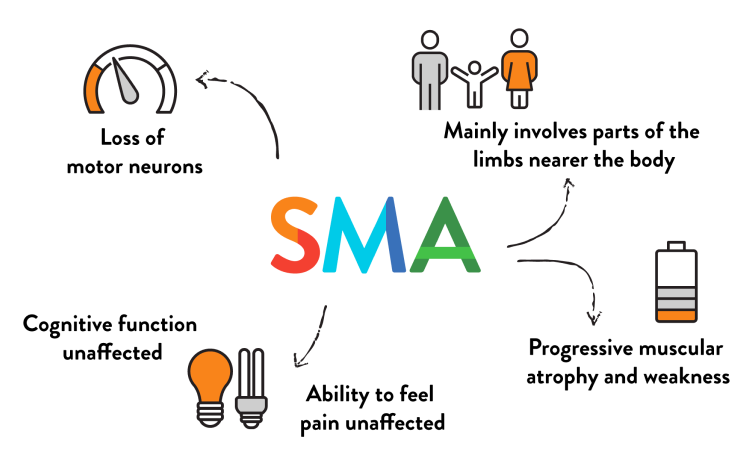
Key characteristics
Loss of motor neurons
Mainly involves parts of the limbs nearer the body (upper arms and thighs)
Progressive muscular atrophy and muscle weakness
Can affect muscles used for feeding, swallowing, and breathing in some patients
Ability to feel pain is unaffected
Cognitive function is unaffected

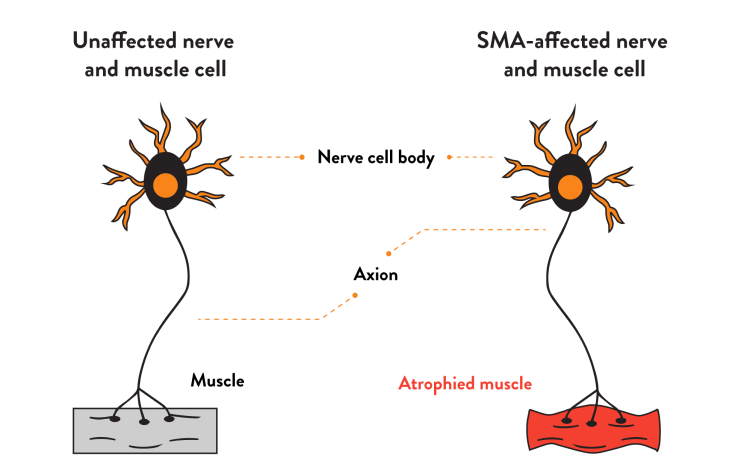

How are nerves affected in SMA?
Motor neurons are nerve cells that control muscle movement and strength by sending signals from the central nervous system (CNS) to muscle cells.
In SMA, as motor neurons deteriorate, muscles stop receiving signals from the CNS, and symptoms such as progressive muscle weakness and decreasing muscle mass (called atrophy) develop.
Understand SMA
What causes SMA?
SMN1 gene mutation
SMA is a genetic disorder caused by a mutation in the survival motor neuron 1 (SMN1) gene which prevents the production of the SMN protein necessary to maintain healthy motor neurons.



The role of genetics in SMA
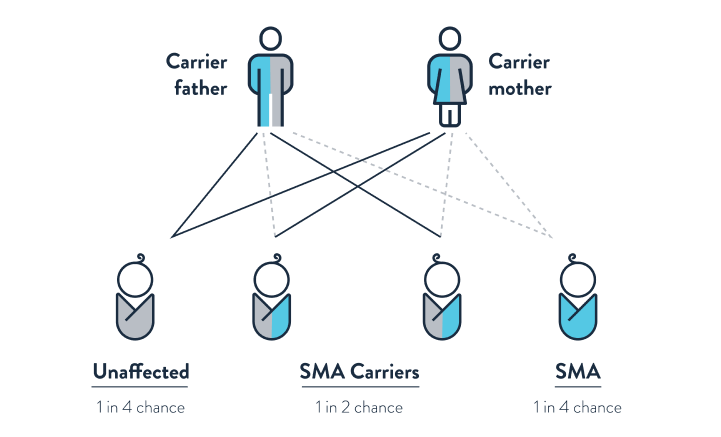
SMA is passed to a child when both parents are SMA carriers and exhibit no signs or symptoms. It is estimated that between 1 in 25 and 1 in 50 people are SMA carriers.
Understand SMA
Signs and symptoms
SMA affects muscle strength and movement. Symptoms can vary greatly depending on age and severity of the condition, with weak muscles around the shoulders, thighs, and hips being the most affected. Breathing and swallowing may also be impacted in some individuals.
Are there different types of SMA?
SMA is a condition with a single spectrum and 5 different types, based on the age of symptom onset and the level of functional ability achieved. SMA types 1, 2 and 3 are most common, however, up to 25% of individuals cannot be accurately classified into a type. Type 0 occurs before birth.



Understand SMA
SMA Questions
Understanding SMA can mean asking a lot of questions. We have provided starter questions for information about SMA, and suggestions for questions you might like to ask your doctor to understand more about SMA.
Approximately 1 in every 10,000 people are born with SMA.1
1. D'Amico A et al. Spinal muscular atrophy. Orphanet J Rare Dis. 2011;6:71.
Approximately 95–98% of SMA diagnoses are cause by mutations to the SMN1 genes.1 This is known by neurologists and researchers as “5q SMA”. There are other, rarer, forms of SMA that may have similar symptoms. A neurologist will include these other conditions in their differential diagnosis.
1. Prior TW et al. Spinal muscular atrophy. NCBI Bookshelf Website. Available at https://www.ncbi.nlm.nih.gov/books/NBK1352/ (Accessed February 2023).
The time until symptoms first appear can vary according to SMA type, but the genetic mutations that caused SMA are present before birth. SMA type 4 is an adult-onset form of SMA and symptom onset is generally around 30 years of age.1
1. Farrar MA et al. Emerging therapies and challenges in spinal muscular atrophy. Ann Neurol. 2017;81(3):355-368.
SMA carriers do not have signs and symptoms of SMA. The only way to determine SMA carrier status is with a genetic test.
It is thought that approximately 1 in 35 people are SMA carriers.1,2 However, individuals with a family history of SMA may have an increased risk of being an SMA carrier.
In making reproductive decisions, it may be helpful to consult with your physician to learn what mutation(s) are common in your family, and what appropriate tests may be required to detect these. Once your family mutation(s) are known, an appropriate test for your situation may be determined.
References:
1. Butchbach M. Front Mol Biosci 2016; 3: 7.
2. Kaczmarek A et al. Expert Opin Investig Drugs 2015; 24: 867–81.
If both parents are SMA carriers, there is a 1 in 4 chance their child will have SMA. It may be helpful to consult your doctor about reproductive decisions and whether SMA carrier screening would be useful.
References:
1. Faravelli I et al. Nat Rev Neurol 2015; 11: 351–9.
2. Lunn MR and Wang CH. Lancet 2008; 371: 2120–33.
1. Faravelli I et al. Nat Rev Neurol 2015; 11: 351‑9.
2. Lunn MR and Wang CH. Lancet 2008; 371: 2120‑33.
3. Cure SMA. Understanding SMA. https://www.curesma.org/wp-content/uploads/2020/08/08262020_Understanding_SMA_vWeb.pdf.Accessed: February 2023.
4. Wang CH et al. J Child Neurol 2007; 22: 1027‑49.
5. Rossoll W and Bassell GJ. Results Probl Cell Differ 2009; 48: 289‑326.
6. Butchbach M. Front Mol Biosci 2016; 3: 7.
7. Kaczmarek A et al. Expert Opin Investig Drugs 2015; 24: 867‑81.
8. Munsat TL and Davies KE. Neuromuscul Disord 1992; 2(5‑6): 423‑8.
9. D’Amico A et al. Orphanet J Rare Dis 2011; 6: 71.
10. Farrar MA et al. Emerging therapies and challenges in spinal muscular atrophy. Ann Neurol. 2017;81(3):355‑368.
11. Kolb S and Kissel J. Neurol Clin 2015; 33: 831‑46.
9 more references
You may also be interested in
A diagnosis of SMA is made with the help of genetic testing. Children and adults with SMA share a similar diagnostic journey.
Every individual with SMA may experience symptoms and the effects of SMA differently. Care options are tailored to the needs of each individual.